More Information
Submitted: March 25, 2025 | Approved: April 04, 2025 | Published: April 07, 2025
How to cite this article: Mishra M, Mulsange K, Rathod1 G, Konda D. Clinical and Histopathological Mismatch: A Case Report of Acral Fibromyxoma. Arch Pathol Clin Res. 2025; 9(1): 005-007. Available from:
https://dx.doi.org/10.29328/journal.apcr.1001045.
DOI: 10.29328/journal.apcr.1001045
Copyright License: © 2025 Mishra M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Acral fibromyxoma; CD 34; SMA; S-100
Clinical and Histopathological Mismatch: A Case Report of Acral Fibromyxoma
Monica Mishra1*, Kailas Mulsange2, Gunvanti Rathod1 and Deepthi Konda2
1Pathology Department, AIIMS, Bibinagar, India
2Dermatology Department, AIIMS, Bibinagar, India
*Address for Correspondence: Monica Mishra, Pathology Department, AIIMS, Bibinagar, India, Email: [email protected]
Background: Acral Fibromyxoma (AFM) is a rare benign soft tissue tumour which is described as a fibromatous and myxoid tumour of skin and soft tissue.
Case details: A 40-year-old male presented to the Dermatology outpatient department with swelling over the wrist of one year duration. The swelling was associated with mild pain, and it gradually increased in size to reach its present size. Cutaneous examination revealed a 2x2 cm mobile, cystic to firm, non-tender swelling over the dorsum of the right wrist. Based on its location and clinical features, it was provisionally diagnosed as a ganglion cyst and excision biopsy was done. Histology showed stellate-shaped cells in a myxoid background with round to oval nuclei having a small, inconspicuous nucleolus. Acral fibromyxoma presents a distinct histopathology including a myxoid stroma and spindle-shaped cells, which are essential for accurate diagnosis and management.
Acral Fibromyxoma (AFM) is a rare soft tissue tumour which is a fibromatous and myxoid tumour typically arising in the Acral regions likes digits, wrist joint but rare locations can be ankles, legs with a male predilection exact incidence is not well documented but it is thought to be very uncommon compared to other soft tissue tumours [1]. The tumour is more frequently observed in adults, though rare cases also involve the ankles and legs; the tumour shows male predominance and older adults It is characterized by a unique histopathology and molecular genetics that can aids in its diagnosis and differentiation from other fibromatous neoplasms of skin and soft tissue but still molecular genetics is not well studied [2]. The tumour is characterized by a myxoid stroma and a proliferation of spindle-shaped cells. Recent immunohistochemical studies have shown that these tumours typically express markers such as CD34, which aids in distinguishing them from other soft tissue tumours [3-5]. Local recurrence has been found in 22% - 24% of cases but malignant transformation has been not been reported but to low grade malignant tumour may be possible but AFM generally has favourable prognosis with benign course [1,4]. A thorough literature study revealed that few cases has been reported with this clinical and histopathology mismatch.
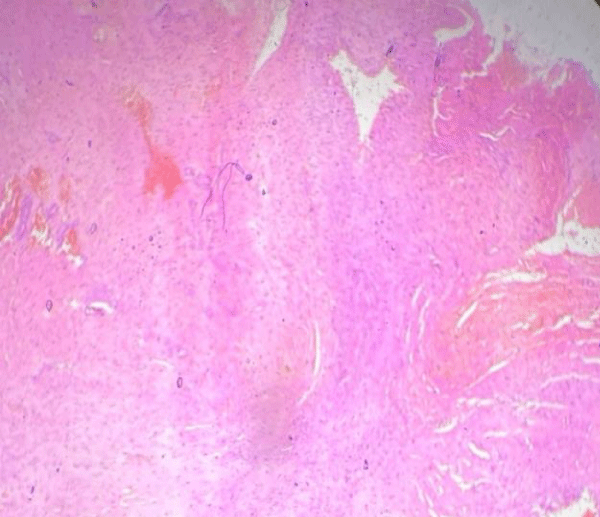
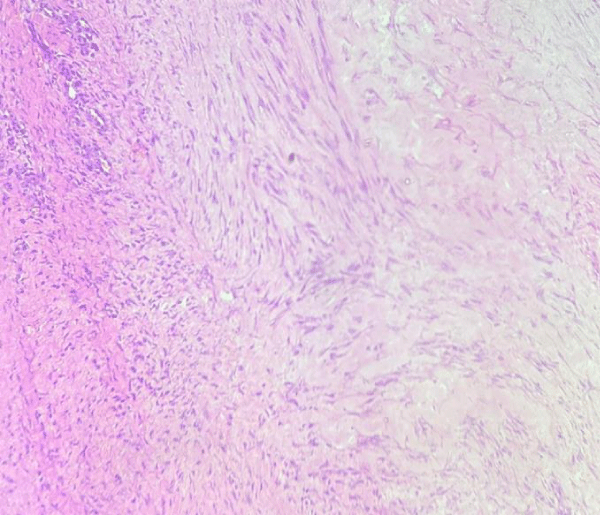
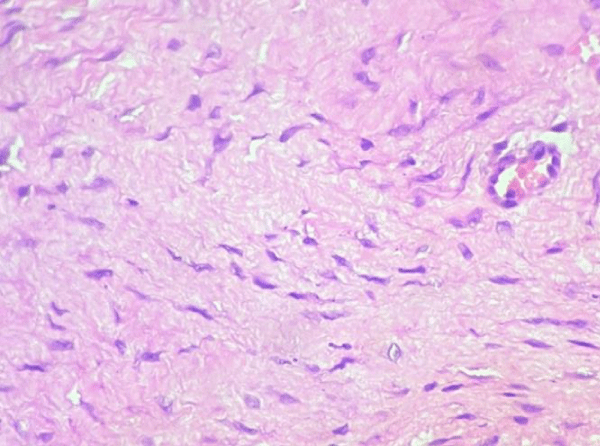
A 40-year-old male presented to the Dermatology outpatient department with swelling over the wrist persisting for one year . The swelling was associated with mild pain, and it gradually increased in size to reach its present size. Cutaneous examination revealed a 2x2 cm mobile, cystic to firm, non-tender swelling over the dorsum of the right wrist. (Figure 1). Based on its location and clinical features, it was provisionally diagnosed as a ganglion cyst and excision biopsy was done. Microscopy showed a poorly circumscribed tumour. The individual tumour cells are stellate-shaped cells with oval to spindle nuclei, with a few cells showing small, inconspicuous nucleoli in a myxoid background (Figures 2-4) . Patient is on follow up but there has been no recurrence for the past year. A final diagnosis of AFM was made after ruling out differential diagnoses including other differentials including myxoid neuromas, superficial angiomyxoma, DFSP, and glomus tumour.
Figure 1: Gross image showing 2x2cm lesion at the wrist.
Figure 2: H & E: poorly circumscribed tumor.
Figure 3: H & E 4x: showed stellate shaped cells in a mxyoid background.
Figure 4: H & E 40×:stellate shaped cells in myxoid background.
AFM often presents as a painless, firm, solitary, sometimes pedunculated mass. AFM typically occurs in distal limbs like fingers and toes. Less common sites are palms, soles, wrists, hands, and thighs. The exact etiology and predisposing factors are not well established [1]. Recent studies emphasize the importance of imaging techniques like MRI for better characterization of the tumour, although definitive diagnosis usually requires clinical, histopathological examination, and immunohistochemistry [3,5]. The tumour follows a benign course with a recurrence rate of 22% - 24%, and no case has been reported showing malignant change [1]. The matrix of AFM contains a mucin-rich, gelatinous stroma with a proliferation of spindle-shaped cells. The tumour typically exhibits a well-circumscribed, non-encapsulated growth pattern. Its hallmark is a loose, gelatinous myxoid matrix. That provides a striking contrast to the densely cellular components [3]. The spindle cells are often arranged in a storiform pattern and are interspersed with small blood vessels. These bland nuclei and minimal pleomorphism aid in differentiating AFM from sarcomas . This feature helps to differentiate AFM from more aggressive soft tissue tumours, such as sarcomas [5]. Immunohistochemical staining plays a crucial role in the diagnosis of AFM. The tumour cells typically express markers such as CD34, which is indicative of their fibroblastic lineage. Additionally, they may also show positivity for smooth muscle actin (SMA) in some cases, reflecting myofibroblastic differentiation. However, they typically lack expression of S100, desmin, and cytokeratin, helping to rule out nerve sheath and epithelial tumours , which helps rule out other potential diagnoses such as dermatofibroma or nerve sheath tumours [2,5].
The histopathological features of acral fibromyxoma necessitate careful differentiation from other soft tissue tumours, including dermatofibromas, myxofibrosarcomas, and other fibromyxoid lesions. The myxoid stroma and the specific cellular arrangement are key aspects that pathologists consider in making an accurate diagnosis. The absence of significant nuclear atypia and the presence of the characteristic myxoid matrix are crucial points that help to distinguish AFM from more aggressive tumours [2].
Recent studies have identified genetic mutations, particularly in the loss of the RB1 gene, associated with acral fibromyxoma. While genetic testing is not routinely performed in clinical settings, it may eventually offer additional diagnostic and therapeutic avenues [2,3]. Understanding the pathological features of AFM is essential for effective management. Complete surgical excision is the primary treatment modality, and the prognosis is generally favourable. However, patients should remain under follow-up due to reported recurrence in up to 25% of cases. Careful histopathological evaluation is critical, as incomplete excision can lead to recurrence, reported in up to 25% of cases [2].
AFM is characterized by distinct histopathological features such as myxoid stroma and spindle-shaped cells, which are essential for accurate diagnosis and management. Immunohistochemistry like CD 34 is not diagnostic or unique to AFM but requires combination of clinical, histomorphology. A better understanding of its genetics may enhance diagnostic precision and may provide potential therapeutic strategies, however, further research is needed to establish genetic markers and definitive diagnostic criteria for AFM.
- Tan HL, Ahmad TS, Sankara Kumar C, Khirusman Adnan Y, Looi LM, Gunasagaran J. Superficial acral fibromyxoma: insights from case management and comprehensive literature review. EFORT Open Rev. 2024 Feb 1;9(2):129–137. Available from: https://doi.org/10.1530/eor-23-0151
- Dehner CA, Pearson H, Almohsen SS, Lo YC, Thangaiah JJ, Torres-Mora J, et al. Acral Fibrochondromyxoid Tumour: A Clinicopathologic and Molecular Genetic Study of 37 Cases. Mod Pathol. 2024 Dec;37(12):100599. Available from: https://doi.org/10.1016/j.modpat.2024.100599
- Goo J, Jung YJ, Kim JH, Lee S Yul, Ahn SK. A case of recurrent superficial acral fibromyxoma. Ann Dermatol. 2010;22(1):110–113. Available from: https://doi.org/10.5021/ad.2010.22.1.110
- Debordes PA, Hamoudi C, Weingertner N, Di Marco A. Superficial acral fibromyxoma: a case of missed diagnosis. J Surg Case Rep. 2023 Feb 1;2023(2):rjad027. Available from: https://doi.org/10.1093/jscr/rjad027
- Fetsch JF, Laskin WB, Miettinen M. Superficial acral fibromyxoma: a clinicopathologic and immunohistochemical analysis of 37 cases of a distinctive soft tissue tumour with a predilection for the fingers and toes. Hum Pathol. 2001 Jul;32(7):704–714. Available from: https://doi.org/10.1053/hupa.2001.25903