More Information
Submitted: February 06, 2025 | Approved: February 10, 2025 | Published: February 11, 2025
How to cite this article: Azzakhmam M, Allaoui M, Elochi R, Elktaibi A, Oukabli M. Hepatic Angiomyolipoma Mimicking Hepatocellular Carcinoma: Another Rare Case Report Arch Pathol Clin Res. 2025; 9(1): 001-004. Available from:
https://dx.doi.org/10.29328/journal.apcr.1001044.
DOI: 10.29328/journal.apcr.1001044
Copyright License: © 2025 Azzakhmam M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Epithelioid angiomyolipoma; Immunohistochemistry; Liver
Hepatic Angiomyolipoma Mimicking Hepatocellular Carcinoma: Another Rare Case Report
M Azzakhmam*, M Allaoui, R Elochi, A Elktaibi and M Oukabli
Department of Pathology, Military Hospital Mohamed V of Rabat, Morocco
*Address for Correspondence: M Azzakhmam, Department of Pathology. Military Hospital Mohamed V of Rabat, Morocco, Email: [email protected]
Epithelioid angiomyolipomas (AML) are uncommon mesenchymal neoplasms, belonging to the group of perivascular epithelioid cell neoplasms (PECOMA). Hepatic PECOMA is even rarer. It’s difficult to diagnose in preoperative by imaging, especially when the fatty component is scant or absent. The gold standard for the diagnosis is histologic examination coupled with an immunohistochemical study. Positive HMB45 immunostaining of the myoid cells is a major diagnostic feature. Herein, we report a particular case of hepatic angiomyolipoma in a middle-aged woman with no significant medical past history. The preoperative diagnosis was difficult given the absence of specific clinical manifestations, even the radiologists considered high suspicion of hepatocellular carcinoma. The final diagnosis has been made by post-operative histology coupled with an immunohistochemistry study.
Angiomyolipomas (AML) are a group of rare mesenchymal tumors, belonging to the group of Perivascular Epithelioid Cell neoplasms (PECOMA). These rare lesions are mostly encountered in the kidney; hepatic PECOMAs are even rarer. The hepatic location is the second most common site of AML [1-5]. These tumors have particular tissue composition: they are composed of blood vessels, smooth muscle, and adipose tissue in varying proportions. This particularity makes it hard to distinguish hepatic AML from other liver tumors [1,3]. In many reported cases, such as ours, it can present similarly to malignant tumors, in particular hepatocellular carcinoma, clinically and radiologically [6]. This makes the preoperative diagnosis too difficult, as it is reported to be less than 25% [3,5,7]. Preoperative diagnosis of HAML is based on radiological examination. However, given the variability of their growth pattern, various proportions of tissue components, and their proximity to major hepatic vascular structures, they are highly misdiagnosed. Histological analysis using immunohistochemical testing, particularly the positive staining for human melanoma black 45 (HMB45) and smooth muscle markers, remains the cornerstone for confirmation diagnosis [8,9,10].
The patient was a middle-aged woman, 35 years old, with no significant medical history except a history of anemia and an ovarian cyst, confirmed to be benign in histology. A tomography was realized during a usual medical checkup for nonspecific abdominal pain and led to the discovery of a lesion of the liver on abdominal.
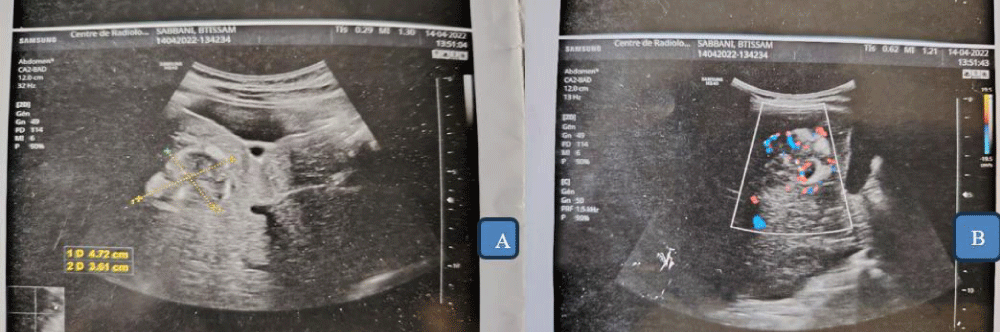
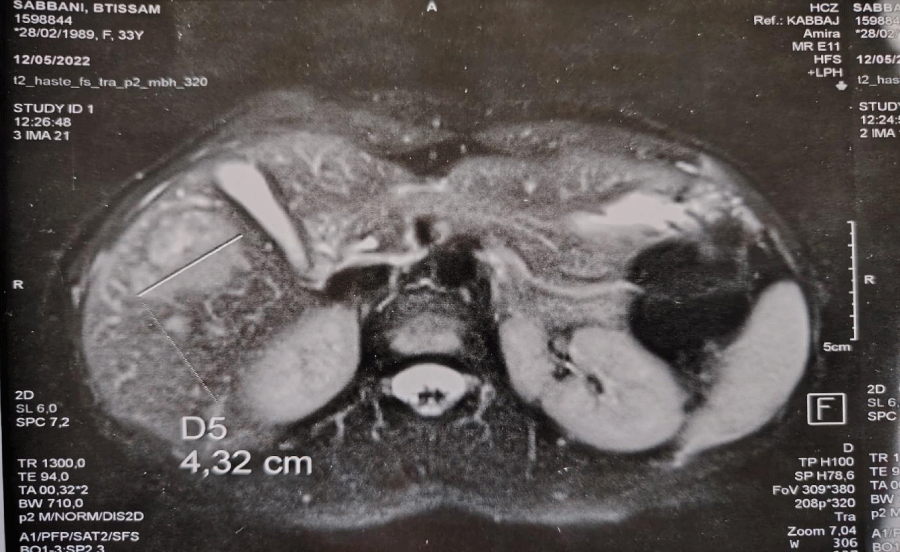
This exam found a heterogeneous tissular formation of 47x36mm, in the V hepatic segment, well-vascularized in Doppler (Figure 1). This suspicious morphological aspect gives the need to perform abdominal magnetic resonance imaging (Figure 2). The liver was of normal size, with a lesion of multiloculated aspect, located on segment V measuring 4,32cm with low intensity observed in the T1-weighted image and high intensity in the T2-weighted image. As a result, the MRI aspect makes diagnosis suspicion of an adenoma or hepatocellular carcinoma.
Figure 1: A. Hepatic tomography showing a heterogenous lesion on the segment V. B. The lesion is Well vascularized on Doppler.
Figure 2: Abdominal MRI showing a multiloculated lesion leading to suspect a diagnosis of hepatic adenoma or carcinoma.
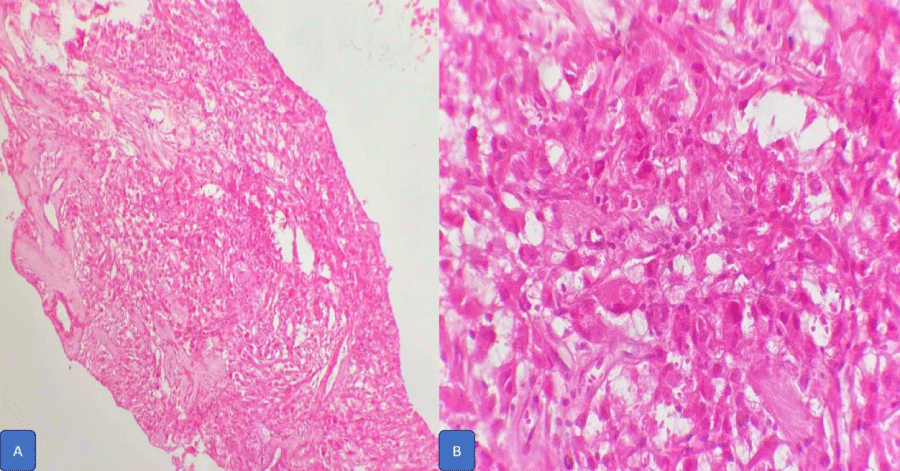
The patient underwent a fine-needle biopsy of the hepatic mass and histopathological examination found a triphasic proliferation pattern made of scanty mature lipomatous components associated with myomatous spindle cell proliferation and capillaries of thick wall. All component shows no atypical cytomorphology or mitosis.
The histological evaluation of the biopsy specimen revealed a storiform fusiform cell neoplasm with expansive borders, areas of a myopericytomatous pattern, and the presence of rhabdoid cells. The neoplastic cells, spindled to oval, with eosinophilic and granular cytoplasm and with mild nuclear atypia, were organized in small bundles (Figure 3).
Figure 3: The pleomorphism of histological features of hepatic angiomyolipoma is shown (A: ×100, B|: x400 H&E stain) (adipose tissues, foam cells, smooth muscle cells).
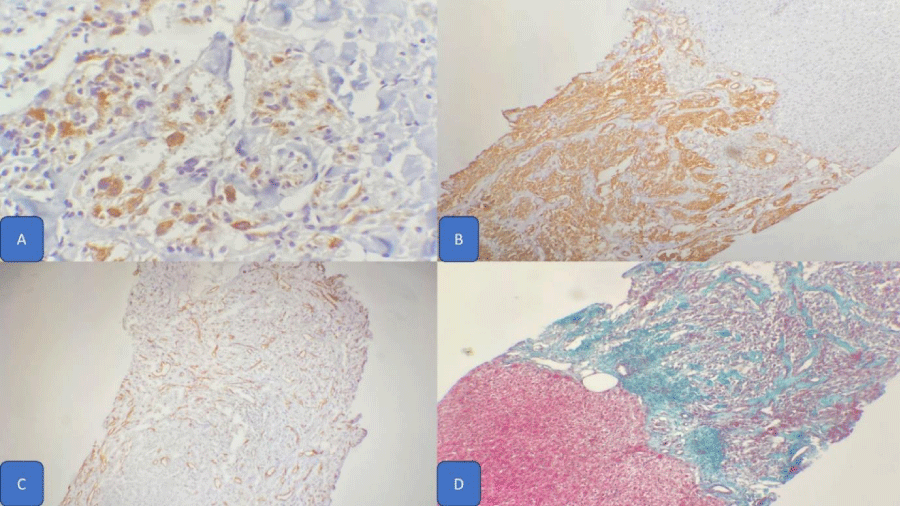
Anomalous arterial structures have been observed too. The immunohistochemical study revealed immunoreactivity of neoplastic cells for SMA and HMB45, S100, and CD31 (Figure 4).
Figure 4: Immunohistochemical study showing expression of HMB45 (A) and SMA (B) by tumoral cells, and CD31 by endothelial cells of vascular component (C) The trichrome special coloration (D) intralesional fibrosis with well-circumscribed borders with adjacent normal liver parenchyma. (HEx20).
The trichrome special coloration (D) intralesional fibrosis with well-circumscribed borders with adjacent normal liver parenchyma (HEx20).
Thus, contrary to the preoperative diagnosis of hepatocellular carcinoma, the morphological aspects and the immunohistochemical profile favored the diagnosis of epithelioid angiomyolipoma.
Hepatic angiomyolipomas belong to the group of Epithelioid perivascular Cells of malignant potential [1-5,11,12]. In 2013, the World Organization for Health defined PECOMAs as mesenchymal tumors composed of distinctive cells that show a focal association with blood vessel walls, and usually express melanocytic and smooth-muscle markers [13,14]. The most common site of occurrence is the kidneys. Hepatic AML is even rarer and more than 200 cases of HAML have been reported in the English language literature so far. The age of diagnosis ranges from 10 to 80 years [12,15], and our patient was 35 years old. AML is frequently associated with tuberous sclerosis, particularly in the kidney AML is reported to be in more than 20% of patients. In contrast, hepatic AML is associated with tuberosis in less than 6% of patients [14,15]. In our patient, there was no medical history of tuberous sclerosis. In most reported cases, patients with HAML were asymptomatic and their tumors were found incidentally as in our patient. No helpful laboratory tests for this disease are known. Hepatitis markers were negative, and liver function was normal.
Imagery is a helpful tool to establish or even to guide the diagnosis. The imagery features depend on the AML composition of tissue, specifically of the variable amounts of intralesional fat (from < 10% to more than 90%), smooth muscle, and proliferating vessels present [13,15].
The perfect imaging technique to detect the fat macroscopically and microscopically is the MRI [10-15]. Lesions with abundant fat components are hypointense on T1 and T2 weighted MRI sequences [15]. This fact explains why lesions with abundant fat and vessels are easier to distinguish from other tumors. On the other hand, fat-poor lesions are more difficult to differentiate from hepatocellular carcinoma. In our case, the fat component was scanty giving the rise of malignancy suspicion in imagery. Radiologists could not exclude the eventuality of a hepatocellular carcinoma.
Histologically, hepatic AML is composed of a variable mixture of fat, vessels, and smooth muscle cells [1,6,7]. Another commonly present component, although not necessary for diagnosis, is hematopoietic tissue. It should be emphasized that the SMCs are the only specific and diagnostic component of hepatic AML and are characteristically positive for HMB-45 and Melan-A [12,14]. These lead to the distinction of four histological subtypes of smooth muscle cells within the AML: spindle, intermediate, epithelioid, and pleomorphic cells [6,10,15,16].
The lipomatous AML type is the most common type, the tumor is composed then of at least 70% lipomatous tissue [10-15]. The myomatous subtype has as much as 10% adipose tissue. Another reported type is the lipomatous and angiomatous type composed predominantly of vascular and lipomatous structures [12]. Each type is composed of a heterogeneous mixture of three types of cells, the most important being the SMCs. Tumors that are composed predominately of myomatous elements (myomatous subtype) are the type most likely to cause diagnostic confusion.
The pathognomonic feature of angiomyolipoma is the positivity of smooth muscle cells for HMB45 along [12,14,15] with the positivity for muscle markers. In our case, HMB45 and Smooth Muscle Actin showed diffuse strong positive staining, the CD31 was expressed by endothelial cells of the vascular wall (Figure 4).
The main differential diagnosis of epithelioid angiomyolipoma is hepatocellular carcinoma or hepatocellular adenoma [9,17-20]. There was no expression of alpha foetoprotein, nor cytokeratin 7 and 20.
Through this case report, we confirm the importance of considering hepatic AML, as a major differential diagnosis that can easily mimic hepatic carcinoma. Our report is in agreement with most published studies even case reports or series studies [1-9,13-20]. The HAML, as it shows no specific clinical symptoms, nor radiological signs. Furthermore, biological tumor markers remain every time within the normal range [16]: the main diagnostic tools remain histological analysis coupled with immunohistochemical studies. It should be considered in every case of hepatic tumor suspicion; histological analysis of the tumor sample must consider the HAML as a potential differential diagnosis, and the immunohistochemical panel must include related antibodies.
In conclusion, hepatic epithelioid angiomyolipomas can lead to considerable diagnostic problems clinically, radiologically, and pathologically because of their diverse morphology. Diagnostic confusion arises when the fat cell component is inconspicuous and the smooth muscle component assumes an unusual morphologic phenotype. The diagnostic difficulty escalates in a fine-needle aspiration setting as was the case in our patient since the biopsy specimen is not representative of the entire tumor. Histopathological diagnosis is relatively easy on the surgical specimen with adequate sampling of the lesion. The striking feature in our case was the unusual macroscopic appearance of the tumor mimicking a vascular neoplasm. The possibility of angiomyolipoma should be considered whenever unfamiliar hepatic tumors are encountered.
Informed consent
Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article. The authors declare that this report does not contain any personal information that could lead to the identification of the patient. The paper has been published after total consent of the patient.
Consent for publication
All authors contributed to the design and interpretation of the study and to further draft and approve the final version to be published.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors.
- Limaiem F, Baccouch S, Boujelbene N, Atallah A, Hajri M, Gabsi S, et al. Puzzling hepatic tumor: Epithelioid angiomyolipoma. Clin Case Rep. 2022;10:e05327. Available from: https://doi.org/10.1002/ccr3.5327
- Tsui WMS, Colombari C, Portmann BC, Bonetti F, Thung SN, Ferrell LD, et al. Hepatic angiomyolipoma; a clinicopathologic study of 30 cases and delineation of unusual morphologic variants. Am Surg Pathol. 1999;23:34-38. Available from: https://doi.org/10.1097/00000478-199901000-00004
- Nonomura A, Mizukami Y, Kadoya M, Matsui O, Shimizu K, Izumi R, et al. Angiomyolipoma of the liver: its clinical and histological diversity. J Hepat Bil Surg. 1996;3:122-132. Available from: https://link.springer.com/article/10.1007/BF02350921
- Nonomura A, Mizukami Y, Muraoka K, Yajima M, Oda K. Angiomyolipoma of the liver with pleomorphic histologic features. Histopathology. 1994;24:279-281. Available from: https://doi.org/10.1111/j.1365-2559.1994.tb00524.x
- Maebayashi T, Abe K, Aizawa T, Sakaguchi M, Ishibashi N, Abe O, et al. Improving recognition of hepatic perivascular epithelioid cell tumor: case report and literature review. World J Gastroenterol. 2007;21:5432-5441. Available from: https://doi.org/10.3748/wjg.v21.i17.5432
- Yeh CN, Chen MF, Hung TC, Chen TC, Chao TC. Angiomyolipoma of the liver. J Surg Oncol. 2001;77:195-200. Available from: https://doi.org/10.1002/jso.1094
- Nonomura A, Enomoto Y, Takeda M, Takano M, Morita K, Kasai T. Angiomyolipoma of the liver: a reappraisal of morphological features and delineation of new characteristic histological features from the clinicopathological findings of 55 tumours in 47 patients. Histopathology. 2012;61(5):863-880. Available from: https://doi.org/10.1111/j.1365-2559.2012.04306.x
- Goodman ZD, Ishak KG. Angiomyolipomas of the liver. Am J Surg Pathol. 1984;8:745-750. Available from: https://doi.org/10.1097/00000478-198410000-00003
- Lee SJ, Kim SY, Kim KW, Shin YM, Kim HJ, Lee JS, et al. Hepatic angiomyolipoma with minimal fat, mimicking hepatocellular carcinoma. Clin Mol Hepatol. 2012;18(3):330-335. Available from: https://doi.org/10.3350/cmh.2012.18.3.330
- Jeon TY, Kim SH, Lim HK, Lee WJ. Assessment of triple phase CT findings for the differentiation of fat-deficient hepatic angiomyolipoma from hepatocellular carcinoma in non-cirrhotic liver. Eur J Radiol. 2010;73:601-606. Available from: https://doi.org/10.1016/j.ejrad.2009.01.010
- Xu PJ, Shan Y, Yan FH, Ji Y, Ding Y, Zhou ML. Epithelioid angiomyolipoma of the liver: cross-sectional imaging findings of 10 immunohistochemically-verified cases. World J Gastroenterol. 2009;15(36):4576-4581. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2752004/
- Lhommel R, Annet L, Bol A, Gigot JF, Sempoux C, Mathieu I, et al. PET scan with 11C-acetate for the imaging of liver masses: report of a false positive case. Eur J Nucl Med Mol Imaging. 2005;32(5):629. Available from: https://doi.org/10.1007/s00259-004-1698-3
- Kumasaka S, Arisaka Y, Tokue A, Higuchi T, Nakajima T, Tsushima Y. A case of multiple hepatic angiomyolipomas with high (18) F-fluorodeoxyglucose uptake. BMC Med Imaging. 2014;14:17. Available from: https://doi.org/10.1186/1471-2342-14-17
- Xie L, Jessurun J, Manivel JC, Gigot JF, Sempoux C, Mathieu I, et al. Hepatic epithelioid angiomyolipoma with trabecular growth pattern: a mimic of hepatocellular carcinoma on fine needle aspiration cytology. Diagn Cytopathol. 2012;40(7):639-650. Available from: https://doi.org/10.1002/dc.21703
- Yang X, Lei C, Qiu Y, Shen S, Lu C, Yan L, et al. Selecting a suitable surgical treatment for hepatic angiomyolipoma: a retrospective analysis of 92 cases. ANZ J Surg. 2018;88(9):e664-e669. Available from: https://doi.org/10.1111/ans.14323
- Teng D, Xu Y, Meng Q, Yang QS. Unveiling the mystery of hepatic epithelioid angiomyolipoma: A unique case report with literature review. SAGE Open Med Case Rep. 2025;13:1-7. Available from: https://doi.org/10.1177/2050313x251314072
- Tababi R, Medhioub M, Soussi I, Noomen I, Kallel Y, Yakoubi M, Ben Mohamed A, Mahmoudi M, Gharbi G, Bouassida M, Chelbi E, Bouzaidi K, Khsiba A, Hamzaoui ML. Hepatic Angiomyolipoma: A Case Report and Literature Review. J Investig Med High Impact Case Rep. 2024;12:1-7. Available from: https://doi.org/10.1177/23247096241306542
- Calame P, Tyrode G, Weil Verhoeven D, Félix S, Klompenhouwer AJ, Di Martino V, et al. Clinical characteristics and outcomes of patients with hepatic angiomyolipoma: A literature review. World J Gastroenterol. 2021;27(19):2299-2311. Available from: https://doi.org/10.3748/wjg.v27.i19.2299
- Velasco-Albendea FJ, Gil-Belmonte MJ, Estébanez-Ferrero B, Fuentes-Porcel O, Nievas-Soriano BJ. A case report of hepatic angiomyolipoma, inflammatory subtype. Clinico-pathological characterization: a diagnostic challenge. Diagn Pathol. 2023;18:57. Available from: https://doi.org/10.1186/s13000-023-01343-7
- Yoon J, Park SH, Ahn SJ, Shim YS. Atypical Manifestation of Primary Hepatocellular Carcinoma and Hepatic Malignancy Mimicking Lesions. J Korean Soc Radiol. 2022;83(4):808-829. Available from: https://doi.org/10.3348/jksr.2021.0178