More Information
Submitted: September 24, 2024 | Approved: September 30, 2024 | Published: October 01, 2024
How to cite this article: George KK, Thomas JC, Sivaram KB, Krishna Prasad T. A Rare Case of Uvulitis Following Endotracheal Intubation Using C- Mac Videolaryngoscope and How To Avoid It Arch Pathol Clin Res. 2024; 8(1): 016-020. Available from: https://dx.doi.org/10.29328/journal.apcr.1001043.
DOI: 10.29328/journal.apcr.1001043
Copyright License: © 2024 George KK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Uvulitis; C-Mac video laryngoscope; Zameer’s grading; Airway trauma
A Rare Case of Uvulitis Following Endotracheal Intubation Using C- Mac Videolaryngoscope and How To Avoid It
Kiran Kuruvilla George1, Jini Chirackel Thomas2, Krishnan B Sivaram1 and Krishna Prasad T*3*
1Department of Anesthesiology, Sri Narayani Hospital and Research Center, Sripuram, Vellore, Tamil Nadu, India
2Department of Geriatrics, Queen Elizabeth Hospital, Adelaide, Australia
3Department of Anesthesiology, Shri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth University, (Deemed to be University), Chengalpattu, Tamil Nadu, India
*Address for Correspondence: Prof. Dr. Krishna Prasad T, Department of Anesthesiology, Shri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth, (Deemed to be University), Chengalpattu, Tamil Nadu, India, Email: [email protected]
Uvular injuries are uncommon after general anesthesia and can result from direct trauma to the posterior part of the soft palate or compression and restriction of blood flow to the uvula caused by the inadvertent placement of the airway or suction devices in the oral cavity. There have been cases of inflammation and ulceration occurring in the midline oropharyngeal structures such as the uvula after general anesthesia with a tube or laryngeal mask airway, even in the absence of direct trauma or infection, presumably due to compression ischemia. While sore throat following general anesthesia is a common symptom, it is important to evaluate any severe or persistent pain to exclude uvulitis. Here we present a case of uvulitis that developed after the insertion of a flexometallic endotracheal tube using the midline technique during C-Mac video laryngoscopy. We also emphasize the measures that can be implemented to prevent such a complication.
The entrapment of the uvula during intubation often goes unnoticed due to limited oral space after insertion of the video laryngoscope blade, with the intubating anesthetist staying focused on the monitor. This complication following the use of a C-Mac video laryngoscope has not been previously documented.
Among the different complications of general anesthesia described, inflammation of the uvula is a rare occurrence. However, its occurrence is associated with significant morbidity to the patient due to cough, and soreness of the throat and can be even life-threatening especially in pediatric patients in rare situations due to the obstruction of the narrow airway [1]. The Mallampati scoring system quickly became a routine preoperative physical exam to predict the difficult airway [2]. For difficult airways as in Malampatti grade 3 and above, there is poor visualization of airway anatomy necessitating the use of difficult airway assistance devices through the mouth to facilitate tracheal intubations. C-Mac video laryngoscopy device from Karl Storz assists in difficult airway intubations due to the curved D-shaped laryngoscopy blade with a portable high-definition monitor for easy visualization of airway anatomy. The hyperangulated blade avoids neck extension during intubation making it ideal to use in situations where neck injuries are present to avoid cervical spinal cord injuries. But these devices by their nature of being bulkier than standard laryngoscope blades (Macintosh) and different insertion techniques may cause direct trauma or inadvertent placement of the endotracheal tube over the uvula for the duration of the operation thereby causing uvular ischemia and edema, especially in the hands of novice anesthetists. Video laryngoscopy with a Macintosh blade (Storz VLS) showed a better overall satisfaction score, intubation time, and number of intubation attempts [3]. In our study, we propose a method to avoid this unwarranted iatrogenic complication in patients while using a Karl Storz C- Mac video laryngoscopy device [4].
A 30-year-old male patient presented to the emergency department with an alleged history of accidental burns while working on an electric post. He had 2nd-degree non-circumferential full-thickness burns on his right forearm, lower back, and right lower limb with the former and latter being the entry and exit points. Additionally, he suffered neck trauma from a fall off a fifteen-foot ladder. There was no history of loss of consciousness, ear bleeding, signs of head injury, or breathing difficulty. Upon presentation, he was conscious, oriented, and able to move all four limbs. However, he did experience neck pain.
Following initial resuscitation and considering the cervical and lower back symptoms, a CT scan of the brain, cervical and whole spine was performed. This revealed a hematoma collection in the posterior aspect of the neck and upper back, a tear of the interspinous ligament in the cervical and upper thoracic region, and a small chip fracture of the C7 vertebral body along with a layer of prevertebral fluid collection from C1 to C5. There were no signs of compression or spinal cord injury. Additionally, CT scans of the thorax and abdomen showed normal findings.
A neurosurgery consultation was requested, and the patient’s neck was stabilized using a hard collar. Subsequently, the patient was scheduled for emergency wound debridement and collagen application by a plastic surgeon.
A pre-anesthetic checkup was conducted, revealing that he had a moderate build and was well-nourished. He presented with tachycardia with a heart rate of 112 beats per minute, along with normal blood pressure and saturation values. During airway examination, it was noted that the patient had restricted mouth opening due to neck pain. He was categorized as having a difficult airway with a Mallampatti score of grade IV, although mask ventilation parameters were normal. Once the patient was stabilized and it was confirmed that no immediate neurosurgical intervention was required, he was scheduled for surgery under general anesthesia.
Due to the patient’s neck injuries, conventional laryngoscopy with a Macintosh blade was avoided to prevent additional trauma to the cervical spinal cord. Instead, it was determined to intubate the patient using the Karl Storz C-Mac video laryngoscope with a 3-size D- D-blade employing the Manual inline neck stabilization technique (MILS).
Following 3 minutes of preoxygenation, antisialagogue agent glycopyrrolate 0.2 mg and fentanyl 100 ug was administered. Anesthesia induction was achieved with propofol 120 mg and muscle relaxation was facilitated with succinylcholine 100 mg. To maintain proper head positioning and prevent unwarranted neck extension, an assistant secured the patient’s head to the operating table by placing his hands on either side.
The D-blade of the Karl Storz C-Mac video laryngoscope was then inserted using the midline technique for Endotracheal tube insertion, passing through the center of the mouth above the tongue. A styletted 8.0 cuffed flexometallic tube was guided through the vocal cords under direct visualization. Subsequently, the scope was removed and the tube was secured to the right side of the mouth.
The surgical procedure lasted approximately 2 hours and required positional changes from supine to left lateral to access the burned areas. Intraoperative parameters remained stable, and following surgery, the patient’s paralysis was reversed using myopyrolate (neostigmine 5 mg and glycopyrrolate 0.2 mg). He was extubated while fully conscious and then transferred to the recovery room for monitoring.
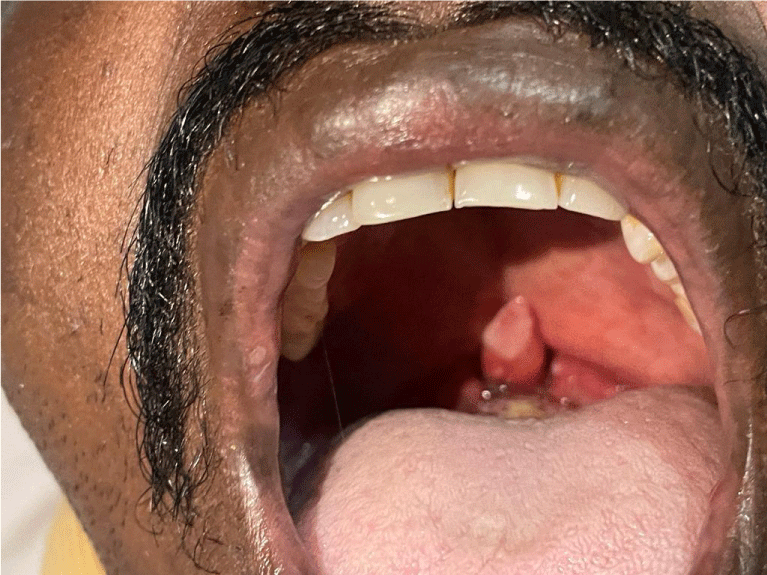
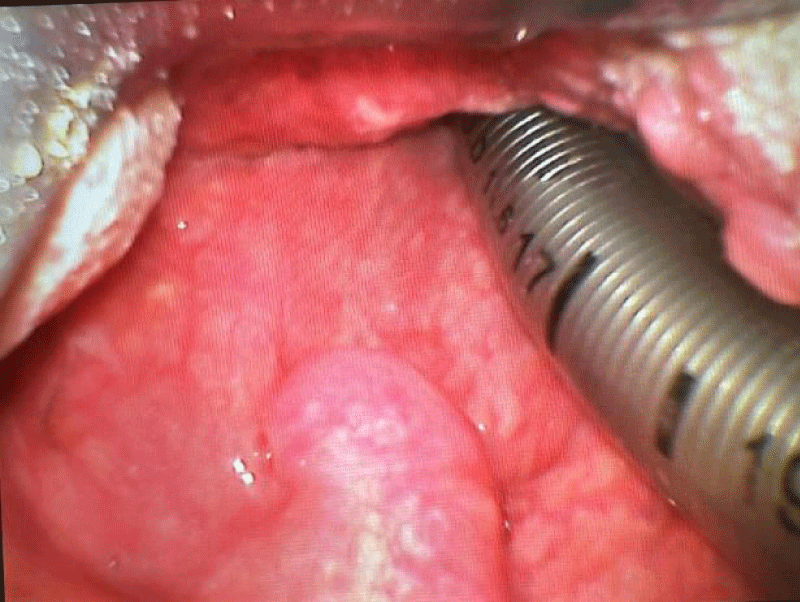
After spending 30 minutes in the recovery room, the patient reported soreness in the throat and odynophagia. He described a sensation of a lump in the throat that worsened gradually. Upon examination using a torch light, the uvula was observed to be inflamed, elongated, and edematous (Figures 1,2). However, there were no signs of airway obstruction, stridor, or breathlessness. He felt comfortable in a 45-head propped-up position. A diagnosis of uvulitis was made, and the patient was closely monitored to ensure no worsening of symptoms. Treatment was initiated, including antihistamines (Pheniramine maleate 25 mg iv twice daily), steroids (Dexamethasone 8 mg iv twice daily), saline gargles, and analgesics with paracetamol and NSAIDS (Diclofenac 75 mg iv twice daily). Additionally, broad spectrum-antibiotic coverage (Cefoperazone and sulbactam 1.5 gm iv twice daily) was continued as per the operative protocol.
Figure 1: Elongated and edematous uvula post extubation.
Figure 2: Uvula with ecchymotic patch reducing in size from Day 2.
The patient underwent regular reassessment and observation to rule out deterioration in symptoms, uvular necrosis, or respiratory complications. An Ear, Nose, and Throat specialist was consulted, and based on their recommendation, the patient was transferred to the Intensive Care Unit (ICU) for overnight observation. Over the next few days, his symptoms improved gradually, and by the third day, the uvula returned to its normal size.
The uvula is a component of the midline soft palate within the oral cavity, aiding in diverting food away from the nasal cavity and towards the oesophagus, as well as playing a role in phonation [1].
While uvulitis is an uncommon complication following general anesthesia, it has been documented after various procedures such as endotracheal intubation, laryngeal mask airways, fiberoptic intubation, transesophageal echocardiography, endoscopy, use of airway patency devices and airway suctioning [5]. Factors like recent upper respiratory tract infections and chronic smoking may predispose individuals to uvulitis, with a higher reported incidence in males compared to females [6]. Airway edema may follow burns injuries and inhalation of smoke particles. Additionally, the use of oral Ring Aldwin Eyer (RAE) tubes and nasal intubation may increase the risk of uvulitis due to the midline placement of the tube [7]. Furthermore, the patient’s surgical position and the duration of the procedure can also contribute to the development of uvulitis.
In most cases, uvulitis following general anesthesia occurs due to the uvula (soft palate) being compressed against a hard surface by the inadvertent placement of oral equipment for various medical purposes [8]. The uvula being a vascular structure, can become edematous, ecchymotic, ulcerated, or even necrotic when compressed for an extended duration, leading to reduced blood flow.
Patients typically exhibit symptoms such as a feeling of a foreign object in the throat, which can result in dysphagia, pain while swallowing (odynophagia), halitosis, and in severe cases, dyspnea or rarely complete airway obstruction, especially in pediatric patients with narrower airways [9]. Diagnosis is usually made through direct examination of the oral cavity.
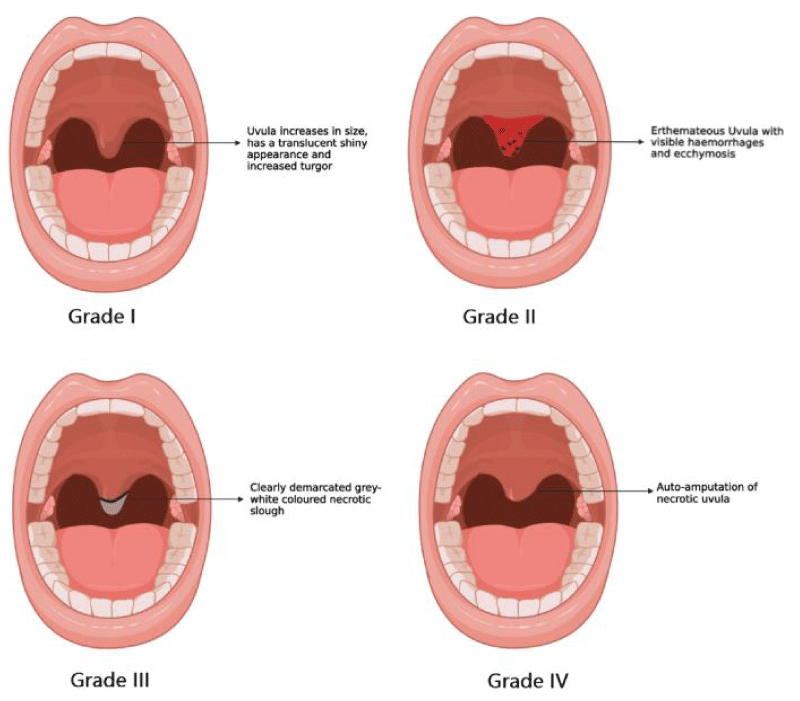
Uvulitis can present in four grades, categorized based on its visual appearance following a traumatic event, as outlined in Zameer’s classification [1] (Figure 3).
Figure 3: Zameer’s classification of Uvulitis [1].
Our patient was categorized as grade 2 uvulitis, characterized by an erythematous uvula with visible hemorrhages and ecchymosis.
Management strategies include reassuring the patient, maintaining a head-propped-up position, antihistamines, steroids, lozenges, mouth gargles, broad-spectrum antibiotics, and arranging for an Ear, Nose, and Throat (ENT) evaluation. In cases of airway obstruction, reintubation may be necessary. Close monitoring of the patient, particularly within the first 24 hours, is crucial to ensure the resolution of symptoms. In rare instances of uvular necrosis, self-amputation of the uvular tip can occur. Surgical intervention, such as excision or microsurgical reconstruction, may be necessary in very rare cases.
While uvulitis cannot be completely avoided, several measures can be taken to avoid its incidence. These include scheduling surgeries after upper respiratory infections have completely resolved, ensuring direct visualization of the oral cavity during suctioning to prevent uvular trauma, maintaining low suction pressure (less than -200 mmHg) [9], and positioning the endotracheal tube to one side of the mouth after intubation.
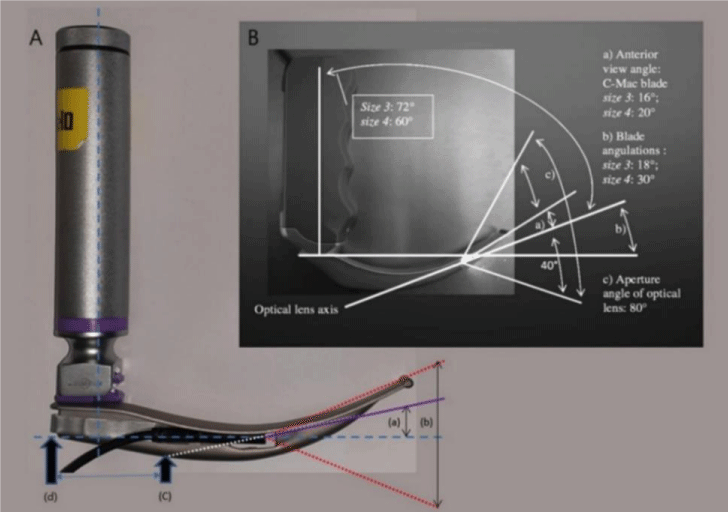
The C-Mac video laryngoscope, initially introduced by Karl Storz in 1999, represents a significant advancement in anesthesia for intubating patients with difficult airways, requiring less effort [10]. Its high-clarity monitor improves visualization ease and facilitates training demonstrations. The advantages of this video laryngoscope include its curved blade at 18° for size 3 and 30° for size 4, offering anterior viewing angles of 16° and 20° respectively, which aids in negotiating difficult airways and reduces the Cormack-Lehane (C-L) grade for glottis visualization (Figure 4). The optic light features an aperture angle of 80°, providing a well-illuminated, clear image of the laryngoscope blade tip and airway anatomy on the monitor as the scope is advanced through the mouth [1].
Figure 4: Comparison of C-Mac video laryngoscope blade with standard Macintosh blade [8].
The technique for inserting the C-Mac video laryngoscope involves inserting the laryngoscope blade through the center of the mouth without sweeping the tongue to the left, while simultaneously visualizing the advancing scope toward the glottis on the monitor. This differs from the standard intubating technique using a Macintosh laryngoscope blade where the blade is introduced through the right side of the mouth and the tongue is swept to the left to obtain a clear view of the glottis before proceeding with intubation.
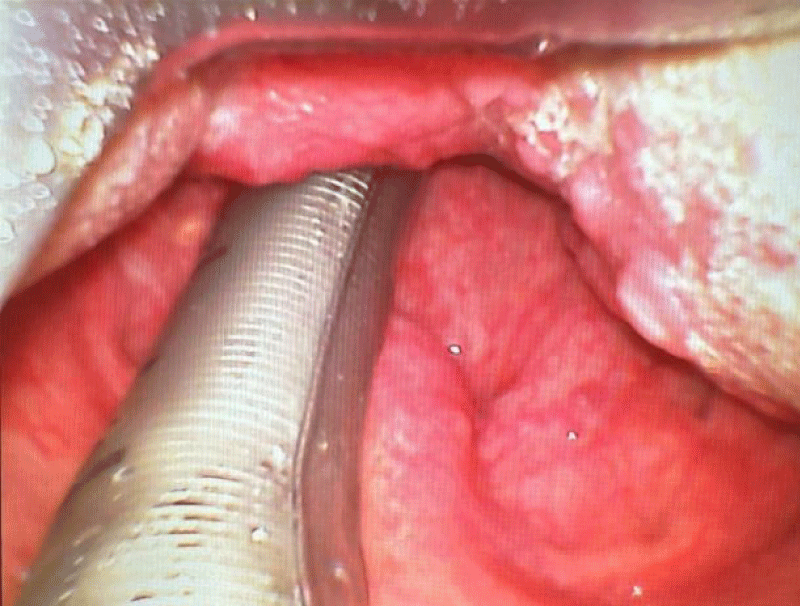
After intubating the patient with the C-Mac video laryngoscope using the midline technique, the tube is secured to either right or left, as depicted in (Figures 5,6). This approach is known as the midline technique for intubation with the video laryngoscope.
Figure 5: ET tube impinging the uvula as seen on video laryngoscope.
Figure 6: ET tube lying free of the uvula as seen on video laryngoscope.
In our patient’s case, the tube was introduced as described above, and we suspect that the cause of uvulitis may be the uvula becoming compressed against the armored tube due to two factors. Firstly, the midline technique of tube introduction with the C-Mac video laryngoscope may predispose the tube to lie over the uvula. Secondly, the failure to effectively displace the tube to one side due to tongue pressure was caused by the premature withdrawal of the video laryngoscope before securing the tube to one side of the mouth.
The limited space in the mouth after inserting the laryngoscope blade and the focus of the intubating anesthetist on the monitor during intubation often leads to the overlooking of uvular entrapment. This is the first reported instance of this complication associated with the C-Mac video laryngoscope.
Recommendations
This complication can be completely prevented by adhering to two straightforward and reliable techniques:
1) Displace the tube to one side of the mouth before retracting the scope, rather than after, to prevent the tongue from pressing against the tube. This allows for unobstructed movement of the tube to one side away from the midline structures of the mouth.
2) Withdraw the laryngoscope slowly from the mouth to look out for real-time, clear visualization of the uvula’s position relative to the tube on the monitor, as demonstrated in Figures 5,6.
In conclusion, this case underscores the importance for anesthetists to be mindful of potential airway injuries, particularly involving the uvula, and to exercise caution during airway instrumentation, including the use of video laryngoscopes. Implementing these straightforward adaptations can help prevent distressing situations for patients and possibly avert potential airway complications, ultimately reducing anesthesia-related morbidities.
Declaration of patient consent
The authors attest that they have all the necessary patient permission paperwork. The patient(s) has/have provided permission on the form for the publication of his/her photos and other clinical data in the journal. The patient(s) is/are aware that their identities and names will not be published, and anonymity is ensured.
Financial support and sponsorship: Self-funded.
- Zameer S, Inam SM, Faisal M, Khan HA, Fatima A, Anwar U. Iatrogenic uvular injury after endotracheal intubation: recommendations for clinical practice. Ain-Shams J Anesthesiol. 2023;15:54. Available from: https://doi.org/10.1186/s42077-023-00351-5
- Mallampati SR. Clinical sign to predict difficult tracheal intubation (hypothesis). Can Anaesth Soc J. 1983;30(3 Pt 1):316-7. Available from: https://doi.org/10.1007/bf03013818
- van Zundert A, Maassen R, Lee R, Willems R, Timmerman M, Siemonsma M, et al. A Macintosh laryngoscope blade for video laryngoscopy reduces stylet use in patients with normal airways. Anesth Analg. 2009;109(3):825-31. Available from: https://doi.org/10.1213/ane.0b013e3181ae39db
- Xue FS, Li HX, Liu YY, Yang GZ. Current evidence for the use of C-MAC videolaryngoscope in adult airway management: a review of the literature. Ther Clin Risk Manag. 2017;13:831-41. Available from: https://doi.org/10.2147/TCRM.S136221
- Emmett SR, Lloyd SD, Johnston MN. Uvular trauma from a laryngeal mask. BJA: British Journal of Anaesthesia. 2012;109(3):468-9. Available from: http://dx.doi.org/10.1093/bja/aes294
- Ziahosseini K, Ali S, Simo R, Malhotra R. Uvulitis following general anesthesia. BMJ Case Rep. 2014;2014. Available from: https://doi.org/10.1136/bcr-2014-205038
- Bright MR, Concha Blamey SI, Beckmann LA, Culwick MD. Iatrogenic uvular injury related to airway instrumentation: a report of 13 cases from the webAIRS database and a review of uvular necrosis following inadvertent uvular injury. Anaesth Intensive Care. 2021;49(2):133-9. Available from: https://doi.org/10.1177/0310057x20982623
- Smith Z, Lobo S. Uvular necrosis in an adolescent following general anesthesia in the prone position. Anaesthesia Cases. 2015;3(1):7-11. Available from: https://doi.org/10.21466/ac.UNIAAFG.2014
- Xue FS, Li HX, Liu YY, Yang GZ. Current evidence for the use of C-MAC videolaryngoscope in adult airway management: a review of the literature. Ther Clin Risk Manag. 2017;13:831-41. Available from: https://doi.org/10.2147/tcrm.s136221
- Cavus E, Kieckhaefer J, Doerges V, Moeller T, Thee C, Wagner K. The C-MAC videolaryngoscope: first experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110(2):473-7. Available from: https://doi.org/10.1213/ane.0b013e3181c5bce5
- Kim JH, Choi JW, Kwon YS. Laryngoscope tracheal intubation education for beginners using a smartphone and a smartphone endoscope. J Coll Physicians Surg Pak. 2020;30(12):1365-6. Available from: https://doi.org/10.29271/jcpsp.2020.12.1365